MINDFUL IN THE CITY
Thoughts
&
Musings
How Do You Know if Therapy is Working?
People come to therapy for a lot of different reasons: depression, anxiety, relationship issues--the list goes on and on. With so many different reasons to seek support, how do you know when therapy is working?
1.You’re trying something different
What’s that saying?
“The definition of insanity is doing the same thing over and over again and expecting a different result.” --Albert Einstein
People usually start coming to therapy when something in their life isn’t working. It can be very easy to keep ourselves stuck in a rut, engaging in the same old ways of coping, just hoping for things to be different. Starting therapy is usually the first step to trying something different. Over time, you might begin to notice that you’re reacting to old situations in new ways.
2.You might start feeling a little bit worse
As weird as it may sound, you might begin to feel a little bit worse after starting therapy. Now, you’re probably asking yourself: why would I sign myself up for feeling worse? You’d be surprised how much of our time we spend on autopilot--completely unaware of how we’re feeling. A part of working with a mindfulness-based therapist is learning how to become more aware of what you’re feeling. Chances are, you’re not necessarily feeling worse, you’re just more aware of how you’re feeling.
3. You’re talking more about your feelings
Some people come to therapy because they have difficulty talking about their feelings. Therapy is not only a great place to become more aware of how you’re feeling, but it is also a great place to practice putting your feelings into words. You may begin to notice that the more you vocalize how you’re feeling in therapy, the easier it becomes in other areas of your life.
4. You’re more accepting of where you’re at
People come to therapy for a lot of different reasons. It can be very easy to put a lot of expectations on ourselves. Remember: change takes time. One way you might notice therapy is working is when you begin to accept where you are at instead of comparing yourself to an idea of where you should be.
5. You’re asking: how do I know therapy is working?
People often have the experience of becoming more self-reflective after starting therapy. It makes sense that you’d eventually want to re-evaluate how things are going with your therapist, what progress you’ve made, and clarify your goals for therapy. If you’re asking this question, chances are therapy is working.
It’s important to highlight again: people come to therapy for a lot of different reasons. How to tell if therapy is working depends on why you started therapy. This is by no means an extensive list but might serve as a conversation starter in your next therapy session.
Next time, we’ll talk about how to tell when therapy isn’t working.
Codependency: How are you thinking? The Role of “Blaming”
In my last blog I spoke about codependency and three unrealistic patterns of thinking – or cognitive distortions – that are common in codependent relationships. To recap: I defined “codependency” as a bond between someone addicted to a substance, or who engages in dysfunctional behavior(s), and their counterpart, or codependent, who enables their dysfunctional or addictive behavior.
The codependent, sometimes called the giver, will do all sorts of things that aggravate or perpetuate the taker’s behavior. And the codependent will often make great sacrifices in the name of “caring”. These include trying to fix their counterpart, care-take them, compensate for their irresponsible behaviors, protect them from the negative consequences of their actions, etc. The giver is fueled to do this because their sense of self: their mood, self-esteem, feelings of well-being, and subsequently their actions, are often contingent on the taker’s current emotional state, words, or behaviors.
The term cognitive distortion is an important element in Cognitive Behavioral Therapy, or CBT. The theory behind CBT is that our thoughts, or cognitions, determine our feelings and behaviors. CBT posits that we all possess, and repeat to ourselves, a default set of automatic thoughts, which can cause problems for us when they are not appropriate to the situation at hand. CBT identifies irrational or exaggerated patterns of thinking – or cognitive distortions -- which go hand-in-hand with these problematic thoughts. They are ways of thinking that that cause people to perceive reality inaccurately. Today, I will highlight one cognitive distortion frequently seen in codependent relationships: Blaming.
Blaming can operate in both members of the relationship, though not always in the same way. A person engages in “blaming” when they hold the other person responsible for their emotional well-being, emotional pain, or even the actions they take. All sorts of interpersonal and intrapersonal problems stem from blaming.
The codependent might say: “He made me feel terrible about myself.”
This kind of blaming is a distortion: no one can make you feel a certain way. Feeling badly about yourself is a feeling stemming from the belief that the negative comments the taker throws at you must be true. After all, your well-being is contingent upon them (or so your believe) and thus you don’t have to take responsibility for your own feelings or your own welfare.
The partner, or taker, might say: “I drink because you nag me all the time.”
This kind of blaming absolves the partner from taking responsibility for their actions. If someone else is to blame for their drinking, for example, they are justified in not putting in the effort and feeling the discomfort associated with changing, or in this case, getting sober.
Because they also believe in the legitimacy of blaming, the codependent might corroborate the taker’s belief that they, the giver, is to blame –in this case for their partner’s drinking. The codependent thus assumes responsibility for the taker’s dysfunctional behavior: they blame themselves for it. The result: the codependent might feel tremendous guilt and work themselves into a pretzel to stop “causing” the taker’s problem.
Here, the blaming is clearly a distortion. It is not realistic to blame yourself for someone else’s dysfunctional behavior. That’s the other person’s responsibility and choice. Taking on the blame again absolves the taker from the responsibility for their own behaviors, and it encourages them to unload their feelings of guilt onto the codependent.
Blaming is not exclusive to codependent relationships either. People have a natural tendency to occasionally blame others for negative situations of their own making to avoid painful feelings like guilt, embarrassment and shame. In a codependent relationship, blaming is the default setting and is corroborated by both parties to distract them from difficult feelings and painful realities. Do you recognize a pattern of blaming in your relationship? If so, the first step to healing is awareness.
Practicing mindfulness moves you towards awareness by helping you see your current reality – your current situation -- more objectively. Difficult as that awareness can feel, psychotherapy supports you in moving towards acceptance of the reality of your situation, which is a necessary step in the healing process. Psychotherapy offers the tools to facilitate change by teaching you to correct your faulty thought patterns. Mindfulness-based psychotherapy provides you the tools and the support to sit with the difficult feelings surrounding your situation without needing to divert attention from them by engaging in faulty thought patterns such a blaming.
According to CBT, when thoughts change, feelings and behaviors change. So when even one partner starts to recognize and sit with the reality of their relationship and the difficult feelings associated with it, they can begin to alter their distorted ways of thinking. They can start to change their behaviors in the relationship, which is bound to disrupt unhealthy dynamics, leaving room to develop healthier patterns and a healthier relationship.
Join me in my next blog where we’ll take a closer look at another cognitive distortion you see in codependent relationships: The Control Fallacy.
Until then!
Codependency: How Are You Thinking?
I work with several clients who say they are codependent or in a codependent relationship. Codependency is defined in a variety of ways by different experts, and plays out differently for different people. Many speak of codependency in close relationships between someone addicted to a substance or behavior and their counterpart (the codependent) who “enables” their addictive behavior. However, a parallel dynamic can also operate in relationships between a codependent person, "the giver" and a non-substance-abusing partner, "the taker", who might possess such qualities as neediness, immaturity, or entitlement or be under-functioning or emotionally troubled.
The codependent, sometimes labeled the giver might try to fix their counterpart, care-take them, compensate for their irresponsible behaviors, protect them from the negative consequences of their actions, etc. These acts of “caring”, often involve making extreme sacrifices for the taker. The codependent enables their partner, rather than allow them to learn to take responsibility for themselves. The codependent’s sense of self: their mood, self-esteem, feelings of well-being, and subsequently their actions, are often contingent on the taker’s current emotional state, words, or behaviors. The codependent believes that their brand of loving and caring is a good thing, even though others can see how unhealthy it is for both parties.
What’s going on for the codependent that keeps them in this dysfunctional pattern? Here are some ideas to consider:
What they are thinking: Cognitive Behavioral Therapy, or CBT, is based on the premise that our thoughts, or cognitions, determine our feelings and behaviors. CBT posits that we all possess, and repeat to ourselves, a default set of automatic thoughts, which can cause problems for us when they are not appropriate to the situation at hand. CBT identifies irrational or exaggerated patterns of thinking – or cognitive distortions. These are not the thoughts themselves, but ways of thinking that that cause people to perceive reality inaccurately. There are at least three cognitive distortions common in codependent relationships:
1. Blaming
2. Control Fallacy
3. Fallacy of Change
I’ll explain these distortions in depth in subsequent blogs, but here’s an overview to get you thinking:
Blaming: When people engage in Blaming, they either blame the other person for their emotional distress and any subsequent actions, or they blame themselves for their partner’s dysfunctional behavior and emotional upset.
Control Fallacy: There are two sides to the Control Fallacy:
A. External Control Fallacy operates when either party believes their problematic behaviors are caused entirely by external forces beyond their control.
B. Internal Control Fallacy, is when a codependent might think they are responsible for and can even control their partner’s negative feelings.
3. Fallacy of Change: A codependent who believes in the Fallacy of Change thinks they are able to change their partner to be who they want them to be and act how they want them to act if they just figure out how to do it. They employ all sorts of indirect and aggressive strategies to change their partner and because their attempts are based on a fallacy, they fail.
In Summary, if you can relate to any of these thought patterns -- if you see codependency in your relationship with someone -- know that this can be a painful situation and at times can feel beyond repair. The good news is that it is not a done deal. You can start by slowing down and increasing awareness of the dynamic you’re entangled in. An example of a practice that helps to increase awareness of your thoughts is mindfulness.
Mindfulness practice and psychotherapy combined can be a way to get in touch with difficult, uncomfortable feelings and make space to accept things as they are rather than viewing reality with a skewed perspective of what’s going on. t’s important to first understand and become more aware of our problematic thought patterns. Once aware, we have the potential to correct those thought patterns, so that feelings and behaviors can change. When one partner’s behaviors change, the other partner can’t help but adjust, and the potential for a new kind of relationship is born.
Stay tuned for my next blog where we’ll take a closer look at Blaming. Until then!
Mindfulness, Psychotherapy, & Your Brain
Mindfulness and meditation are getting so much hype nowadays! The term mindfulness is used in so many different contexts. At a certain point when a word means everything it can seem like it really means nothing. So, what do the practices of mindfulness and meditation actually look like? How does meditation or mindfulness actually promote change? And how is mindfulness relevant to therapy?
We live in a society that is so rushed and encourages us to manage multiple tasks at once. However, research shows: multitasking isn’t a thing our brains are capable of doing and actually decreases our enjoyment in what we’re doing (Park, Xu, Rourke, & Bellur, 2019). With so much societal encouragement to keep doing, it can be hard to slow down. That’s where mindfulness comes in. Mindfulness is the intentional attunement to all parts of our experience: our thoughts, feelings, and sensations in our bodies. Mindfulness is a daily, hourly, minute-by-minute practice.
For some, it might look like noticing your thoughts wandering in a meeting. For others, it might be savoring every bite of a meal--intentionally chewing and noticing all the flavors of your food. Mindfulness might be noticing what’s happening in your body when you’re fighting with your partner and then choosing how to proceed with the conversation--or pausing the conversation for later. It might be noticing you need a stretch break after a morning of working on the computer; or recognizing that tight feeling in your chest relaxes when you call up a friend.
Mindfulness is a unique practice for each individual--just like psychotherapy. Mindfulness-based psychotherapy is a dynamic process that aims to promote awareness of the connection between your thoughts, feelings and physiological responses. At Mindful NYC our clinicians pull from a wide range of tools to support you in being more aware of what is happeninging in your mind and body.
Ok, so if that’s what mindfulness is, what’s meditation? Meditation is also a practice and will look different for each individual. Traditionally, meditation is the seated, formal practice of mindfulness: a meditator will select an allotted time to sit in an upright posture, lower their eyelids, focus on their breath, and notice their thoughts, feelings, and bodily sensations--without judgement.
Research shows that the formal process of meditating actually promotes the micro-practice of mindfulness (Hernández, Suero, Barros, González-Mora & Rubia, 2016). Without getting too scientific: your brain produces electrical impulses all the time--your brain is never not working. What you think about and consciously notice going on around you is only a portion of your whole experience. Your brain is working hard to filter out unimportant stimuli.
When you close your eyes your brain begins to produce more alpha activity. Alpha is associated with calmness and relaxation. When you close your eyes and focus on your breathing: your brain begins to produce more theta activity. We’re still learning so much about the brain, but generally speaking, theta is associated with: relaxed attention, memory/emotional integration, and focus. When we meditate our brains produce more alpha and theta which leads to being more relaxed, aware, attentive, and focused (Lomas, Ivtzan, Fu, 2015).
Over time, the practice of mediation and the neurophysiological processes it promotes changes how your brain processes information and makes it easier to be more mindful (Dentico, et al., 2016). Working with a mindfulness-based psychotherapist is a collaborative process, pulling from a wide range of tools, aiming to connect your mental, emotional, and physical experiences. All-in-all, the combination of mindfulness, meditation, and psychotherapy can help you slow down, relax, and notice more of what’s happening in your mind, body, and environment.
References
Dentico, D., Ferrarelli, F., Riedner, B. A., Smith, R., Zennig, C., Lutz, A. Tottoni, G., & Davidson, R. J. (2016). Short Meditation Trainings Enhance Non-REM Sleep Low-Frequency Oscillations. PLoS ONE, 11(2), 1–18. https://doi-org.tcsedsystem.idm.oclc.org/10.1371/journal.pone.0148961
Hernández, S. E., Suero, J., Barros, A., González-Mora, J. L., & Rubia, K. (2016). Increased Grey Matter Associated with Long-Term Sahaja Yoga Meditation: A Voxel-Based Morphometry Study. PLoS ONE, 11(3), 1–16. https://doi-org.tcsedsystem.idm.oclc.org/10.1371/journal.pone.0150757
Lomas T, Ivtzan I, & Fu, C. (2015). A systematic review of the neurophysiology of mindfulness on EEG oscillation. Neuroscience & Behavioral Reviews, 57, pp.401-410. Retrieved from 10.1016/j.neubiorev.2015.09.018
Park, S., Xu, X., Rourke, B., & Bellur, S. (2019). Do You Enjoy TV, while Tweeting? Effects of Multitasking on Viewers’ Transportation, Emotions and Enjoyment. Journal of Broadcasting & Electronic Media, 63(2), 231–249. https://doi-org.tcsedsystem.idm.oclc.org/10.1080/08838151.2019.1622340
The Importance of Ritual in Self-Care
Self-care has become a wildly popular concept in the last few years, especially in the field of mental health. While everyone has their own views of what constitutes self-care, I like this definition from PsycheCentral: “Self-care is any activity that we do deliberately in order to take care of our mental, emotional, and physical health.”
Despite its wholesome aim, self-care has a darker side. Anne Helen Peterson wrote about the negative effects of the commodification of self-care: “Give yourself a face mask! Go to yoga! Use your meditation app! But much of self-care isn’t care at all: It’s an $11 billion industry whose end goal isn’t to alleviate the burnout cycle, but to provide further means of self-optimization. At least in its contemporary, commodified iteration, self-care isn’t a solution; it’s exhausting.”
Self-care has become a wildly popular concept in the last few years, especially in the field of mental health. While everyone has their own views of what constitutes self-care, I like this definition from PsycheCentral: “Self-care is any activity that we do deliberately in order to take care of our mental, emotional, and physical health.”
Despite its wholesome aim, self-care has a darker side. Anne Helen Peterson wrote about the negative effects of the commodification of self-care: “Give yourself a face mask! Go to yoga! Use your meditation app! But much of self-care isn’t care at all: It’s an $11 billion industry whose end goal isn’t to alleviate the burnout cycle, but to provide further means of self-optimization. At least in its contemporary, commodified iteration, self-care isn’t a solution; it’s exhausting.”
This is the primary problem with self-care: for many, it becomes just another task to squeeze into your schedule. In a society that encourages people to feel productive every moment of the day, it’s a cruel Catch-22: in trying to take care of yourself, you end up feeling guilty--or even more stressed out! Beyond this, many people may not have the funds or the time to schedule regular massages, yoga classes, or even lunchtime walks outside (which points to a much larger conversation about money, power, and privilege).
Given these obstacles, how can we cultivate a form of self-care that truly betters our lives?
The answer can be found in this quote by Evette Dionne, editor-in-chief of Bitch Magazine: “Self-care is not about vacations and bubble baths--no matter what you’ve heard from an Instagram influencer. It’s a set of cultivated habits designed to preserve mental, emotional, and physical health.” The phrase “a set of cultivated habits” denotes that self-care needs to be integrated into our lives in a consistent, fundamental, and ritualistic way.
In a religious context, rituals are routinely-performed ceremonial acts, often in a community setting. In a self-care context, people adopt or create personal rituals for a variety of reasons: to calm, to ground, to set intentions, to feel empowered, to celebrate one’s body, etc. Humans have been performing rituals for at least 70,000 years, but in these busy times, we don’t always make space for the habits we know will nourish us.
Regular practices like yoga, meditation, and therapy are becoming more socially acceptable forms of self-care. And it can be particularly helpful to work with an expert in a self-care capacity, whether that’s a yoga instructor, meditation teacher, or therapist. Experts can help you create a safe space for self-exploration and self-support, as well as discuss ways in which you can further cultivate self-care on your own. When working with any teacher or therapist, it’s important to both take the time to find people who respect your agency and comfort, and to check in with yourself frequently throughout the process.
There are also many types of rituals that can be done on your own. On the podcast Call Your Girlfriend, one of the hosts sets aside her birthday “day” every month to work on items that are important but hard to make time for (create a budget, pay bills, etc.). Some create daily routines that help them take care of their minds or bodies. Ayurvedic practices often include daily practices of self-massage with oil, as well as a focus on the types of foods ingested. All rituals have the common thread of engaging in self care with intention and mindfulness.
As a therapist and yoga teacher, I’ve found that the cycles of the moon are an excellent opportunity to engage in self-care. Each month, the New Moon offers the start of a new cycle in which one can release what’s no longer needed and set intentions for the month ahead. Each New Moon is in a different astrological sign, an opportunity to focus on different areas of one’s life (career, relationships, home, etc.). I’ve led New Moon Circles with a group, but more often I do these practices on my own. Integrating this ritual into my schedule on a monthly basis gives me the opportunity to set aside time to focus on the inner work that I may not have the “time” to do otherwise.
Whatever rituals you choose, the sense of sacred ceremony imbues self-care with an extremely empowering message: my well-being matters. It becomes less about buying products and services, and more about taking the time and space to tune into oneself. Becoming more aware of our inner world is a gentle invitation to deepen our understanding and compassion. It also opens space for us to facilitate changes in other parts of our lives. Therapist Jack Moran stated: “Whenever you make a mindful choice to respond differently than usual, combining awareness with concrete action, your goals and motivations make a leap toward actualization.” Ritual self-care can give us a strong platform with which to move towards that actualization.
Containment: Beginning Trauma-Focused Therapy for Post-Traumatic Stress Disorder
Mindful Psychotherapy Services Director of Education and Training, Bryan Aston explains the essentials of working with post traumatic stress disorder. Mindful will be offering a series of continuing education courses in Spring 2019 to licensed social workers and helping professionals working with trauma interested in learning more about PTSD. This video may also be helpful for clients with a traumatized history to learn more and seek help.
Fear to Power, Power to Fear: Women’s Voices in Group
FCGPS Annual Conference
(more info)
November 10, 2018
10:00am-5:00pm
University of Colorado Health Center
for Dependency, Addiction and Rehabilitation
1693 Quentin Street
Aurora, CO 80045
AGPA Annual Conference
(more info)
February 25 - March 2, 2019
Westin Bonaventure Hotel
404 S. Figueroa Street
Los Angeles, CA 90071
Leaders:
Yoon Kane, LCSW, IFSCP, CGP
Saralyn Masselink, LCSW CGP
"What are the words you do not yet have? What do you need to say?" -Audre Lorde.
Mindful Founder and Executive Director, Yoon Kane LCSW, IFSCP, CGP will be co-leading a full-day institute and a half-day experiential training group with Saralyn Masselink LCSW, CGP in Denver, CO and Los Angeles, CA. This training opportunity for therapists will explore cultural expectations as a ‘passionate bad fit’ for women and ways they are unconsciously repeated in group.
From a young age, women receive messages about how to be nice, compliant, accommodate others, and gain approval, both from the family and the communities they grow up in. These messages arrest women’s natural development of a sense of self-worth and entitlement. There is a dichotomy introduced into young female psyches that sets women up to believe that the cost of being powerful is a loss of connection and belonging.
These culturally-sanctioned beliefs that govern patterns of behavior are unconscious and are played out and repeated in group dynamics. Group also has the potential to encourage people to have new experiences that foster new beliefs and paradigms and offers opportunities to try on and test out fresh ideas and ways of being.
These experiential training workshops will explore questions such as: What are women’s relationships to having power and agency? What does the fear of power communicate about the female self and early relationships with caregivers? How can group provide reparative experiences that counter dysfunctional cultural norms? The group leader can help members become conscious of these limiting dynamics and establish new norms that offer the space for maturational experiences previously limited by socio-cultural conditions.
Be sure to connect with Yoon Im Kane LCSW, PC for questions and discussion. She will be part of the expert panel at the FCGPS Annual conference in Denver, CO Sunday 11/11/18 4:00-5:30pm.
Look forward to seeing you there!
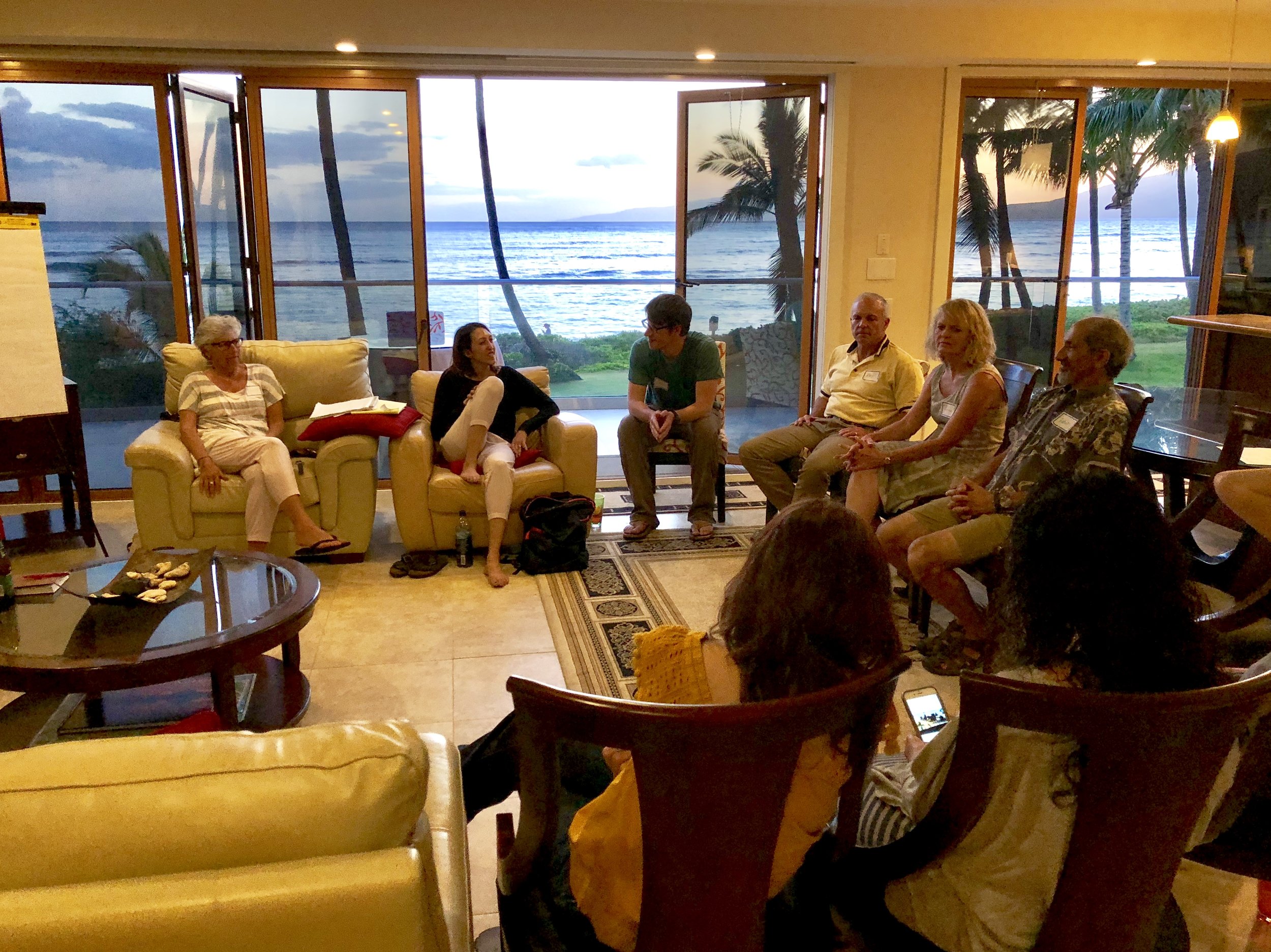
2018 Getting to the Heart of the Matter Mindful Retreat: Intimacy from the Inside Out Experience
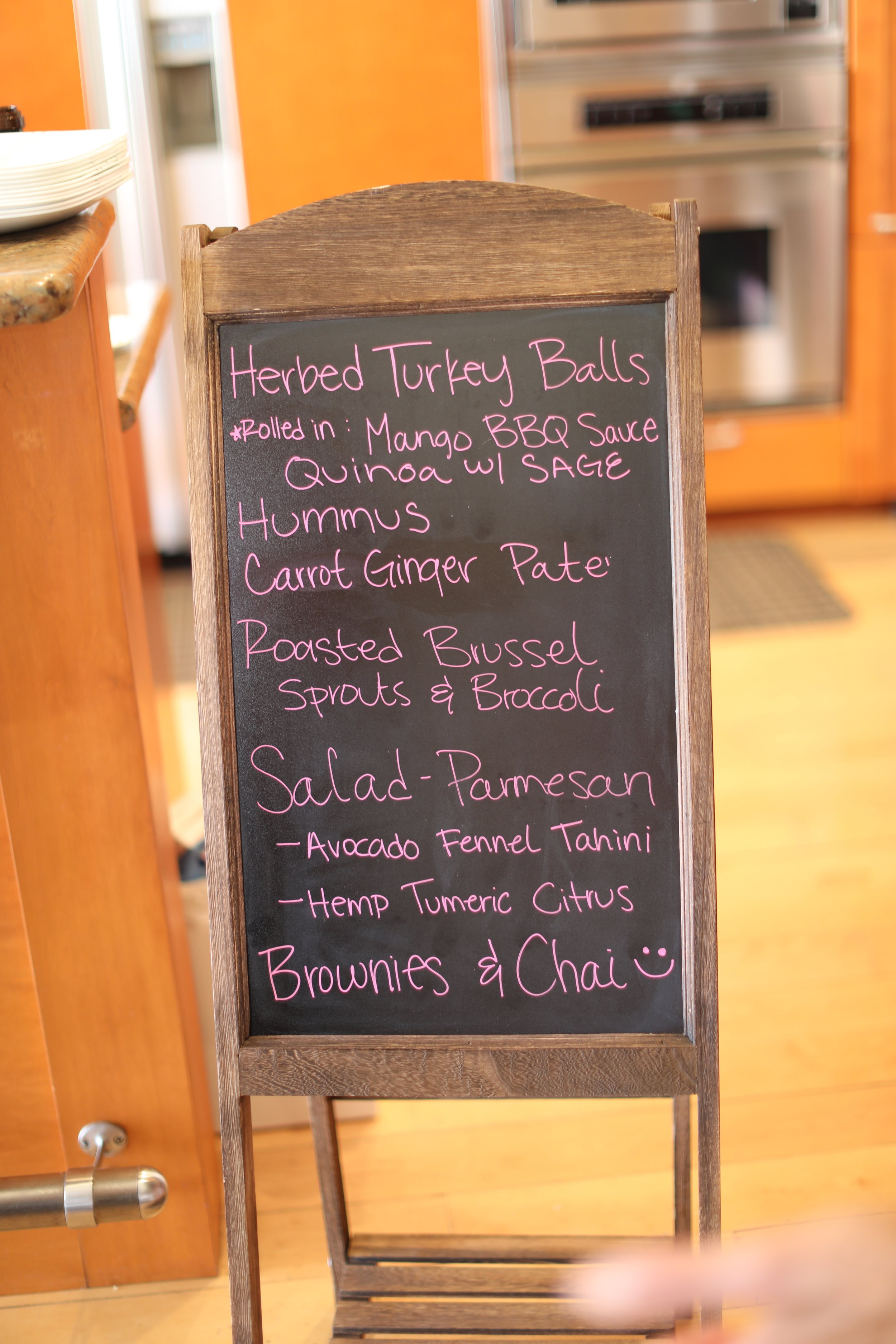
The Getting to the Heart of the Matter Mindful Hawaii retreat was an experience of rejuvenation, relaxation and rediscovery. Toni, Morgan and Yoon were a fantastic team and thanks to Jessica and her crew, we experienced the flavors of Maui in delicious, locally-sourced meals. Not a drop of rain and spectacular sunsets - thank you Hawaii!
The Getting to the Heart of the Matter Mindful Psychotherapy Services Hawaii retreat was an experience of rejuvenation, relaxation and rediscovery. Toni, Morgan and Yoon were a fantastic team and thanks to Chef Jessica and her crew, we experienced the flavors of Maui in delicious, locally-sourced meals. Not a drop of rain and spectacular sunsets - thank you Hawaii!
We arrived as a group of strangers from diverse backgrounds - couples and individuals from New York, Texas, Chicago and California. Maui’s magical sunsets, sea turtles, hikes and beaches deepened our intensive journey of the heart, mind and body. Through yoga, journaling, talking and meditating on the beach, we practiced returning to the self and the heart to allow difficult emotions and settle our protectors.
Giving ourselves the experience of being nurtured and held over five days, gave us the time and space to metabolize and integrate our intellectual learning in a deeper, emotional way. As the days unfolded, we started to sink in and practice new ways of being and connecting with one another moment-to-moment. By getting to understand and accepting the protective parts of us that try to keep us safe, we were able to access our courage and open-heartedness. What a powerful, new way to experience ourselves and each other.



















To Combat Panic Anxiety Think “3-2-1”
In a previous blog, I wrote about different manifestations of anxiety: generalized anxiety, anxiety attacks and panic attacks. At the Mindful Psychotherapy Practice, I often encounter clients who experience one or all of these forms of anxiety, and many of them get great temporary relief from the “3-2-1” exercise.
One of my patients, Janie, just had this kind of experience few weeks ago. She had turned in the final draft of a report she and her team had been working on for months, and it suddenly occurred to her that she might have forgotten to double check one section.
In a previous blog, I wrote about different manifestations of anxiety: generalized anxiety, anxiety attacks and panic attacks. At the Mindful Psychotherapy Practice, I often encounter clients who experience one or all of these forms of anxiety, and many of them get great temporary relief from the “3-2-1” exercise.
One of my patients, Janie, just had this kind of experience few weeks ago. She had turned in the final draft of a report she and her team had been working on for months, and it suddenly occurred to her that she might have forgotten to double check one section. She came into the therapy session wracked with anxiety and worry over this possible mistake, and was overcome with dread and fear about the disastrous consequences, as if she had definitely overlooked that section and conclusively missed something important. She reported to me that she was unable to let the thought go, even though there was absolutely nothing she could do about it until the next day at work. Jumping to negative conclusions and creating worse case scenarios in her head were driving her crazy and contributing to shortness of breath and a racing heartbeat that made her thoughts more intense.
So I taught her one of the most effective mindfulness tools for calming the nervous system, the 3-2-1 exercise:
It’s really simple.
Take a deep breath and name for yourself 3 things you see (e.g. the woman across from you, the advertisement above the railing, the cracked window), then name 3 things you hear, ( the rumble of the train, a child talking, your own breath), then, name 3 things you feel, tactilely (e.g. the hard seat under your backside, your watch on your wrist, and the soles of your feet in your shoes).
Take your time and try to focus exclusively on those things as you name them.
Next, do the same but name two things you see, you hear, then you feel. If you can’t find new ones every time that’s okay, but just really experience them fully as you name them. Finally, name 1 thing in each category.
By the time Janie came into her next therapy session, she reported using the 3-2-1 technique and was surprised to find that her thoughts were no longer spinning. She was able to breathe more calmly, her heart rate slowed and she was able to assess the situation more realistically and redirect her thoughts to calm herself down further (“I can’t do anything about this now, so I will turn on my music and relax”.) Bottom line, Janie used the exercise to ground herself in the present and free herself from racing thoughts that led her to catastrophic and extreme assumptions.
When you feel anxious and unsettled, try the 3-2-1 exercise. It’s also very useful if you have trouble falling asleep, your mind filled with worried preoccupations. At the least, this exercise will ground you in the present. At best, you’ll be able to proceed serenely with your day, or clear your mind and fall asleep.
Author: Kayla Schwartz - LMSW - Clinical Associate
You Are Not Alone: Common Forms of Anxiety
As a psychotherapist practicing in New York City, I’ve treated my share of patients who experience a baseline of anxiety, intermittent anxiety and panic attacks.
What’s the difference between them?
People who have a persistent level of anxiety live with a baseline of excessive, uncontrollable worry about a number of things – and they may anticipate disaster even when the actual events do not merit it. They may experience any or all of the following symptoms: restlessness, fatigue, trouble concentrating, muscle tension or sleep disturbances.
As a psychotherapist practicing in New York City, I’ve treated my share of patients who experience a baseline of anxiety, intermittent anxiety and panic attacks.
What’s the difference between them?
People who have a persistent level of anxiety live with a baseline of excessive, uncontrollable worry about a number of things – and they may anticipate disaster even when the actual events do not merit it. They may experience any or all of the following symptoms: restlessness, fatigue, trouble concentrating, muscle tension or sleep disturbances. When these symptoms persist for more than 6 months and happen more days than not, these people may be eligible for the diagnosis of “Generalized Anxiety Disorder.” When the level of anxiety is mild to moderate people can function fine, though with discomfort. Severe levels of anxiety may cause sufferers to avoid anxiety-provoking situations or have trouble carrying out simple daily tasks.
Then there are those who experience episodes of more severe anxiety or anxiety attacks, which are usually triggered by some sort of stressor (e.g. being late and pressured, public speaking, a difficult conversation with one’s boss, etc.). This level of anxiety may include symptoms such as shortness of breath, racing heart, tightness in the chest, confusion, etc. Usually when the stressor goes away, the symptoms gradually subside.
Panic attacks can be an even more debilitating manifestation of anxiety. They may be a reaction to being exposed to the object of a phobia (e.g. large groups of people in the case of social phobia or riding on the subway in the case of claustrophobia), or to a medical condition which brings on scary symptoms (e.g. mitral valve prolapse or hypoglycemia.) Panic attacks are usually short-lived – 10 minutes on average -- but can produce feelings of intense fear and doom. Symptoms include heart palpitation, dizziness, nausea, shortness of breath, a sense of choking, tingling in the body, chest pains and a fear of actually dying. When panic attacks come out-of-the-blue and regularly, with no apparent trigger, the person often becomes very preoccupied about future attacks and they may avoid situations that they believe trigger them. These people may be eligible for the diagnosis of “Panic Disorder.”
If you suffer from any of these forms of anxiety, you are not alone! According to the Anxiety and Depression Association of America, a whopping 40 million or 18% of Americans over the age of 18 have some sort of anxiety disorder. Not only are you in good company, there is no reason to despair! There are numerous types of effective treatments out there, from a variety of talk therapies, to behavioral strategies, to medication, to all of the above. You might start by contacting a psychotherapist who can help you determine a course of action that works for you. As I mentioned before, you are not alone if you have anxiety, so why suffer alone?
Author: Kayla Schwartz - LMSW - Clinical Associate